Why Gut Issues Are More Common in ADHD and Autism (and what’s really going on)
If you’re autistic, ADHD, or both, and you’ve lived with digestive issues for years – constipation, reflux, abdominal pain, unpredictable bowels – you’re not imagining it (and you’re not the only one).
In my work, I hear these stories every single week. People who’ve been struggling quietly for years, often told it’s stress, your diet, or something they should be able to fix if they tried harder.
But when you look at the research, and when you listen to lived experience, a very different picture emerges.
Gut issues are genuinely more common in ADHD and autism.
And there are real neurological, sensory, and physiological reasons why. They about doing something wrong. It’s about understanding how neurodivergent bodies work.
How common are gut issues in autism and ADHD?
Digestive problems are widely reported in autistic people. Research suggests functional gut disorders affect somewhere between 30–70% of autistic individuals – an enormous range, but consistently higher than in non-autistic populations.
The phrase functional gut disorder is used to describe chronic digestive conditions, despite the absence of visible signs of damage or disease. The most commonly reported symptoms include:
Constipation and / or diarrhoea
Nausea, heartburn and bloating
Abdominal pain and discomfort
Constipation in particular is very common in autism and ADHD. For many people it starts in childhood and continues into adulthood, often without anyone joining the dots.
Despite how common these experiences are, they’re still frequently overlooked or minimised in healthcare settings.
Why are gut issues more common in neurodivergent people?
There isn’t one single cause, but a combination of interacting factors, including:
Genetics
Sensory processing differences
Differences in Interoception (internal body awareness)
Effects of medications
Gut microbiome differences
Greater stress and anxiety
None of this is about blame. It’s about biology and individual experiences.
Interoception: sensing what’s happening inside your body
Interoception is your ability to notice internal body cues such as hunger, thirst. fullness, pain and the urge to go to the toilet.
In ADHD and autism, interoception can be highly variable. Some people have reduced awareness of these cues. Others can experience them very intensely. Many fluctuate between the two, often influenced by stress, fatigue, hormones and sensory load.
To correctly identify a body cue (for example to eat or drink), not only does our body need to pick up on changes in our physical state, it also needs to process that information accurately, in order to respond appropriately. Misinterpretation of signals is more common with neurodivergence, meaning hunger and thirst, for example are often confused. You can read more about this here, in an earlier blog.
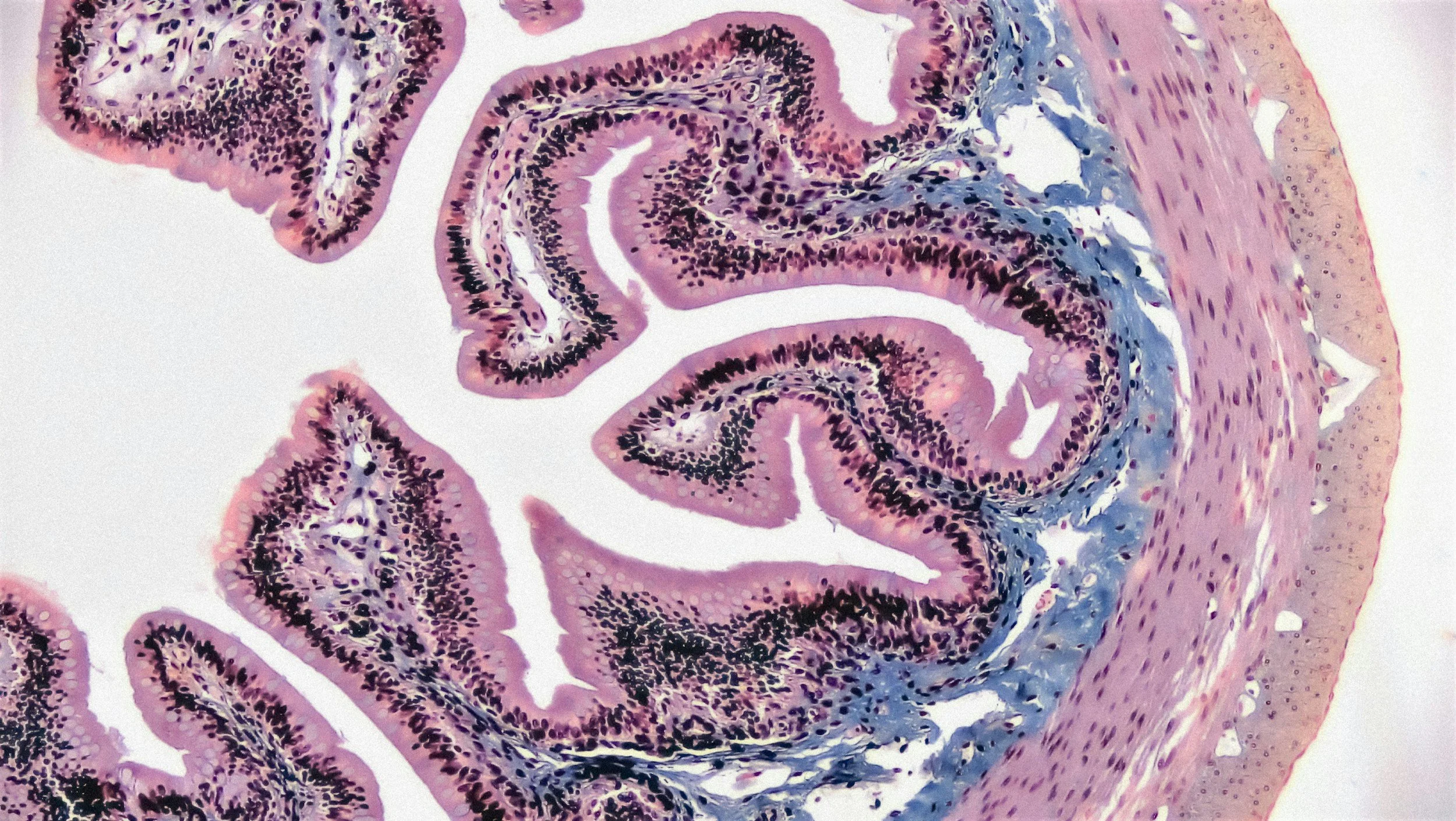
Digestion is a highly sophisticated process that relies on a constant, real-time dialogue between the gut and the brain, known as the gut-brain axis. This system relies heavily on interoception to promote (and stop) eating, coordinate and regulate the muscles of digestion, enzyme secretion and bowel movement, as the body processes food.
Autism, interoception and eating distress.
Many autistic people experience heightened awareness of internal sensations. Hunger, fullness, bloating, pain, or pressure can feel intrusive and distressing.
This can show up as:
Anxiety around food
Strong physical and emotional reactions to eating
Meltdowns or shutdowns driven by physical discomfort
The anticipation of eating in autistic individuals can also differ from the neurotypical experience. In addition to interoception differences, sensory sensitivities and a greater need for routine can elevate anxiety and contribute to rigid food choices and eating behaviours, or conversely, a complete lack of interest in food.
ADHD, Autism and Constipation: what’s really going on?
Constipation isn’t just about fibre or water intake (although those can play a role).
There are several neurodivergent-associated factors I see all the time:
Missing early signals to go to the toilet
Hyperfixation / hyperfocus and time distortion: becoming deeply immersed in something and losing track of time, leading to forgetting to eat, drink or take care of daily necessities.
Getting distracted and forgetting you were heading to the toilet
Avoiding going to the toilet because the environment is overwhelming - echoey, bright lights or strong smells. Then there’s a cold seat, the texture of toilet paper or the feeling of going can be uncomfortable or painful.
Delaying going to the toilet because it feels inconvenient, time-consuming or painful.
Not allowing enough time when using the toilet for pelvic muscles to relax - fidgeting and getting up quickly if nothing happens straight away, leading to incomplete bowel emptying. Over time, incomplete emptying leads to larger, harder stools that are more difficult to pass. The bowel becomes less responsive, and constipation becomes chronic.
This isn’t laziness or poor habits. It’s neurobiology doing its thing – attention, impulse control, sensory processing, and frustration tolerance all interacting.
Anxiety, the nervous system, and the gut
Anxiety is common in both ADHD and autism, and the gut is incredibly sensitive to it.
Chronic anxiety can:
Alter gut motility (movement)
Increase gut sensitivity and pain perception
Worsen reflux and abdominal discomfort
These in turn can further increase anxiety, creating a feedback loop:
Gut symptoms → anxiety → worsened gut symptoms.
Being told to “just relax” or “calm down” is usually unhelpful. It dismisses the individual’s emotional or sensory experience, implying their feelings are wrong, unnecessary, or a choice, rather than an unconscious reaction to overwhelming stimuli or distress. It can feel patronizing and triggering and lead to increased frustration, defensiveness and anger rather than relaxation.
Hormones matter too
For many people I support, gut symptoms shift around hormonal changes – puberty, perimenopause, menopause, and with HRT.
Oestrogen and progesterone influence:
Gut motility
Pain perception
The gut microbiome
So when hormones fluctuate, digestion often does too.
This is especially relevant for autistic and ADHD women, who are already navigating sensory sensitivity, interoception differences, and burnout. It’s another layer that’s frequently missed.
Routines, consistency, and digestive health
Digestive systems love routine. But routines can be challenging with ADHD and autism. When impulsivity is strong, establishing and maintaining routines are often difficult. When routines provide predictability to manage anxiety, rigidity can develop. Even small disruptions in routine can cause surges in anxiety which in turn affects the gut.
Common obstacles include:
Irregular eating patterns (forgetting to eat, or avoiding eating).
Variable energy levels
Executive function challenges
Burnout
When routines fall apart, the gut is commonly affected.
That doesn’t mean routines are impossible. They just need to be:
Realistic
Flexible
Supportive of how your brain actually works
Routines need to be safe, doable, and kind…something is always better than nothing.
Signs your gut issues may be linked to neurodivergence
You might want to explore this connection further if you notice:
Long-standing constipation, reflux, or abdominal pain
Symptoms that worsen with stress or routine changes
Digestive issues that started in childhood
Anxiety around eating or bodily sensations
Feeling disconnected from hunger, fullness, or bowel urges
Standard gut advice hasn’t helped (or made things worse)
Why standard gut advice often doesn’t help
Most mainstream gut health advice assumes:
Consistent routines
Reliable body awareness
Neutral relationships with food
High capacity for planning and follow-through
For many neurodivergent people, these assumptions simply don’t hold.
When advice doesn’t fit your nervous system, it can increase:
Shame
Frustration
Anxiety around food and digestion
A supportive approach starts with understanding how your brain and body interact – rather than forcing yourself into a model that was never designed for you.
A more supportive way forward
There is no one-size-fits-all solution for gut issues in ADHD and autism.
What genuinely helps is:
Working with your nervous system, not against it
Understanding your interoceptive patterns
Reducing shame around symptoms
Making changes that are realistic and sustainable for you
Digestive symptoms in neurodivergent people make sense when you understand the full picture.
You’re not failing at gut health. Your body isn’t being difficult. It’s just communicating differently, and that deserves understanding, not judgement.
I put together this as a useful planner which you may find helpful: Neuro-Affirming Toileting Routine Planner
Mel x